Responding to King v. Burwell: What Policy Levers Can States “Pull” to Maintain Coverage if the Supreme Court Sides with King?
| | Blog, National Health Care Reform
This piece, which addresses the approaches states could consider in the event the Supreme Court eliminates federal marketplace subsidies for certain states, was prepared by Claudine Swartz and Angelique Hrycko of Day Health Strategies and Tom Dehner and Juan Montanez of Health Management Associates (HMA). It was originally published in HMA’s Weekly Roundup on March 4th. DHS and HMA have collaborated on numerous marketplace planning and implementation projects.
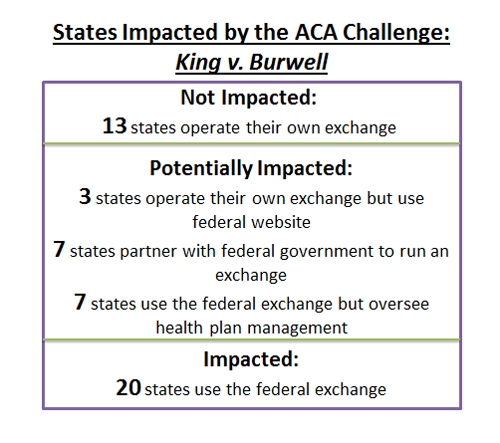
All eyes are on the Supreme Court today as oral arguments in the King v. Burwell case begin. At issue is an IRS rule that authorizes financial subsidies to purchase health insurance offered through the federal marketplace. Unlike the first Affordable Care Act (ACA) challenge that was decided by the Court, which affected the entire country, King v. Burwell is expected to only affect a subset of states. While the case does not involve the 13 states that operate their own exchange, it certainly involves the 20 states that do not operate their own state marketplace and rely on the federal marketplace technology. This leaves us with a gray area, where 14 states have some type of a partnership with the federal marketplace, and 3 states have an established exchange but use the federal marketplace technology to operate it.
Predictions on a court ruling are in full swing. When it comes to the Supreme Court, we endorse the approach of Casey Stengel, who said “I never make predictions, especially about the future.” In fact, the Supreme Court surprised nearly every analyst in 2012 when it used Congress’s taxing authority to uphold the individual mandate, rather than the Commerce Clause. Moreover, while the case appears to simply be about whether federal subsidies are permissible outside of state-established exchanges, there is always the potential for a more complex or nuanced decision, particularly when the political and practical effects of the decision are as sweeping as they are in King v. Burwell.
Leaving predictions aside, it is clear that the potential disruption that could be caused by a lack of subsidized coverage in states using the federal marketplace is significant. A decision to disallow subsidies via the federal marketplace will disrupt coverage for millions of individuals who are currently receiving subsidies (estimates have ranged from 7-13 million), and may negatively influence the operation of state markets for other individual purchasers as well.
Impacted States Should Consider Key Coverage Levers
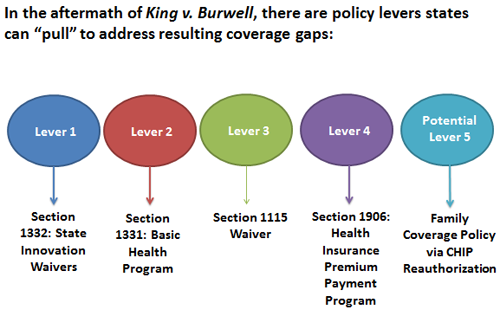
While the King v. Burwell outcome is uncertain, impacted states may begin contingency planning. States can use various levers to protect coverage for individuals that rely on premium subsidies through the federal marketplace. These levers (click image below to enlarge) resemble a calculator full of numbers from the federal code: Sections 1332, 1331, 1115, and 1906.
Lever #1: State Innovation Waivers
State Innovation Waivers have a few different names – Section 1332 Waivers, 2017 Waivers, and the Wyden Waiver – but they all reference the same flexibility: starting in 2017, states have the ability to create an alternative reform framework that results in ACA-comparable coverage levels at no higher cost. States may waive the obligation to operate a health insurance exchange, offer qualified health plans, ensure essential health benefits, provide cost sharing and premium tax credits, and enforce an individual and employer mandate. With federal approval, states could no longer be required to use an exchange – federal or state – to facilitate coverage, while still accessing subsidy funding. The Supreme Court could even look to State Innovation Waivers as a vehicle for states to maintain coverage for individuals that potentially lose subsidies via the federal marketplace. While the waiver submission and approval process is unknown today, this option conceivably provides states the ability to establish a framework to resolve all coverage gaps that may result from a Supreme Court decision, and address a wide range of other issues as well.
Lever #2: The Basic Health Program
While not as far reaching, states can also utilize the Basic Health Program (BHP) – Section 1331 – to provide coverage for individuals with incomes 133-200 percent of the federal poverty level who are accessing subsidies via the federal marketplace. The BHP allows states to offer a coverage program for these individuals principally to minimize churn between Medicaid and exchange coverage. In order to fund a state-based BHP, a state receives 95 percent of the total premium subsidies that would otherwise be spent if coverage were accessed via an exchange.
The BHP is not likely a coverage solution for all individuals receiving subsidies via the federal marketplace, because it does not address those with incomes above 200 percent of the federal poverty level. However, the approach prioritizes the lower-income group of those who could lose access to tax credits, a group that greatly benefits from subsidized coverage and desperately needs it. To date, Minnesota is the only state that has utilized the Basic Health Program, but it could be a tool used more widely in the future.
Lever #3: Section 1115 Waivers
The first two levers are new state tools authorized by the ACA. In contrast, a Section 1115 Waiver has long been used to provide states flexibility within their Medicaid programs and enable ongoing federal funding for state-specific approaches to Medicaid coverage, benefits or delivery systems. This includes using the Section 1115 Waiver is to expand coverage for those ineligible for traditional Medicaid, as was the case when Massachusetts used the Section 1115 Waiver to achieve near universal coverage. Already, states have used Section 1115 Waivers to secure ACA flexibility, with numerous states requesting that Medicaid eligible individuals secure private coverage via a marketplace. In the wake of a Supreme Court decision, states will look to their Section 1115 Waiver authority to examine options to address a new coverage landscape.
Lever #4: Health Insurance Premium Payment Program
In addition to Section 1115 waivers, the Health Insurance Premium Payment Program (HIPP) – Section 1906 – is a well-utilized coverage tool. Here, states may provide financial assistance to income-eligible individuals that select employer sponsored health insurance; in 2011, 24 states had HIPP Programs. This option allows Medicaid funding to be used for employer premiums, deductibles, and co-payments as long as employer coverage is deemed cost effective. While HIPP does not provide states with a complete coverage solution if federal marketplace subsidies are disallowed, it represents one approach that could serve as a piece of an overall solution.
Potential Lever #5: Expanding Family Coverage via CHIP Reauthorization
Last, we turn to a more speculative lever. Federal funding for the Children’s Health Insurance Program (CHIP) expires in 2015. Alongside the reauthorization and funding debate will come the policy suggestion that it may be more efficient and cost effective to cover eligible children through the same health insurance plan as their parents. While we don’t know how, or whether, Congress will address this issue, the door is open for an innovative family coverage policy – particularly if the reauthorization debate is taking place in the context of a changed coverage landscape due to King v. Burwell.
Looking Ahead
Each lever described above varies in its reach and complexity. Some can be deployed in combination for a wider impact. In some instances, the levers are well-known and understood, while others represent new terrain.
If you have questions about the options mentioned here, or want more information about the possible ramifications of the Supreme Court decision, please contact Angelique Hrycko (angelique@dayhealthstrategies.com) at DHS or Tom Dehner (tdehner@healthmanagement.com) at HMA.



Leave a Reply
Want to join the discussion?Feel free to contribute!